Wayne State Doc Publishes Breakthrough Study On Cooling Blanket For Newborns
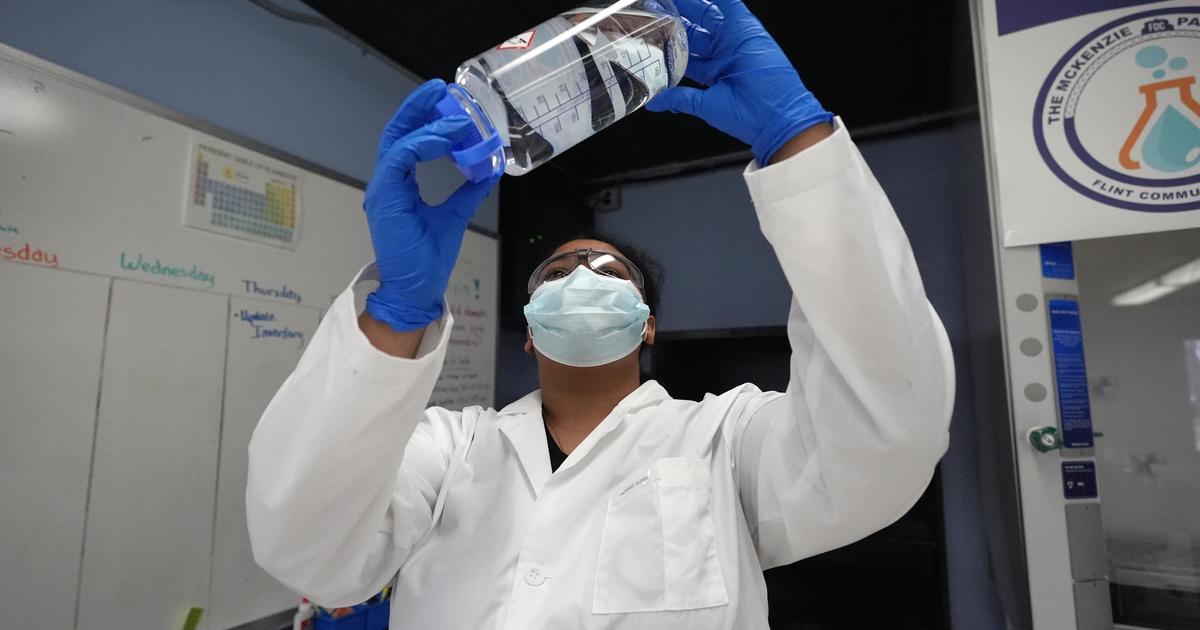
DETROIT -- After more than 10 years of study, investigators in the National Institute of Child Health and Human Development Neonatal Research Network, led by a pediatric researcher at Wayne State University and the Detroit Medical Center, have proven an effective way to significantly reduce death and physical and mental disability caused by reduction in oxygen and blood flow to the brain at birth.
Scheduled to publish May 31 in the New England Journal of Medicine, the study findings will have a "major impact" on the treatment of brain injury among infants born at term with this condition, according to the investigators who conducted the study.
The breakthrough study documented the effectiveness of reducing the "whole-body temperature" of brain-injured newborns during the hours immediately after birth. The initial study, published when the infants were 18 months of age and funded by the Eunice Kennedy Shriver National Institute of Child Health and Human Development, found that the cooling process was successful in significantly lowering the risk of death and physical and mental disability by more than 15 percent among the cooled newborns. The current study shows that the protection of the brain-injured newborns continued without any significant fall-off during the first 6 to 7 years of their lives.
"I don't think there's any doubt that these findings will have a significant impact on the medical treatment of newborns who experience oxygen deprivation at birth," said Seetha Shankaran, M.D., Wayne State University professor of pediatrics and division director of neonatal and perinatal medicine for the DMC Children's Hospital of Michigan and DMC Hutzel Women's Hospital. The study was assembled by Dr. Shankaran, the lead investigator, along with senior study author Rosemary D. Higgins, M.D., program scientist for the NICHD Neonatal Research Network, and 25 other researchers in the NICHD NRN. "This is a very hopeful breakthrough for all of us who work in the field of neonatal medicine," added Dr. Shankaran, who has led the wide-ranging study since its start in 2000.
Titled "Childhood Outcomes after Hypothermia for Neonatal Encephalopathy," the landmark study focused on 208 newborns who had experienced hypoxic ischemic encephalopathy (oxygen deprivation-related brain injury) at birth. During the first phase of the study, conducted between 2003-2005, the cooling treatment of the brain-injured newborns – achieved via a specially designed "cooling blanket" that lowered their whole-body temperature to 92.3 Fahrenheit for 72 hours immediately after birth – resulted in an 18 percent reduction in death and mental disability among the cooled infants, compared to a similar-sized control group that had not undergone cooling but received "usual care." Sixteen percent of the newborns studied were born at DMC Hutzel Women's Hospital and cooled there or transferred to DMC Children's Hospital of Hospital for cooling therapy from other area hospitals. A national multicenter approach was required for the study since many infants with this disorder need to be studied to conclusively demonstrate benefits of a therapy. The NICHD Neonatal Research Network includes 17 academic centers in the United States, who compete every five years for continued participation and funding. The Wayne State University site has been a participant in the Network since its inception in 1985.
Those initial results, based on assessments that were made when the infants were between 18 and 22 months old, was the first study to be performed using the whole-body cooling approach. The study published in 2005 in the New England Journal of Medicine, with Dr. Shankaran as lead author, demonstrated that whole-body cooling was an effective therapy for oxygen-deprived newborns, based on outcomes after 18 months. The current study conducted during the past seven years at 17 different U.S. academic research centers in the NICHD Neonatal Research Network (NRN) continue to track outcomes among the injured newborns through age 7 years. "What's especially relevant about the findings is that there was no significant decline in the rate of improved outcomes among the newborns who received the whole-body cooling," said Dr. Shankaran.
"The results of this randomized trial show indisputably that whole-body hypothermia is an effective treatment for hypoxic ischemic encephalopathy [HIE]," she added. "This is the largest and longest trial of the cooling blanket approach ever performed, and the long-term improvement in outcomes shows that such whole-body cooling is truly a beneficial treatment for this condition."
Describing how the cooling blanket helps protect infants from the effects of HIE, Dr. Shankaran pointed out that infants born at term may fail to get enough oxygen, either from blood loss or from other birth complications. Oxygen deprivation during the birth process, when severe, can result in death rates of up to 60 percent – and survivors often sustain brain damage that can result in cerebral palsy, cognitive impairment or hearing and vision loss. Even if they do not experience detectable brain damage, children who experience HIE at birth are at higher risk for learning disabilities, language delays and memory deficits. (Severe oxygen deficiency at birth is also known as "birth asphyxia.")
By providing whole-body cooling to the infants with HIE during the first 72 hours after birth, the deleterious effects of lack of oxygen and lack of blood flow are slowed down and thus reduce the physiological detrimental effects that accompanies oxygen deprivation.
In the wake of the original study, Dr. Shankaran and several of the other members of the NICHD research team pointed out that neonatal units around the world have adopted this cooling technique to reduce the risk of death and disability among full-term infants who show signs of the brain dysfunction indicating oxygen deficiency. Whole-body hypothermia is now the "standardized treatment" for HIE in brain-injured newborns. In addition, the researchers noted that the current hypothermia therapy is being utilized for treating adult patients who experience oxygen deprivation as a result of heart attacks, strokes, spinal cord injuries and other forms of trauma that injure the brain due to lack of oxygen. It should be noted that the use of hypothermia in adults has not been followed by long term studies showing sustained benefits of cooling therapy.
While assessing that potential, Dr. Shankaran pointed out that "what's especially exciting about our study is that the meticulous long-term follow-up [over seven years] of HIE-affected newborns who received the cooling therapy had never been conducted before. This is the first long-term study of extremely high-risk children who received cooling at birth, and it seems likely that the benefits we documented in newborns may be replicated in adults and pediatric patients undergoing cooling."
The New England Journal of Medicine study concluded on an equally upbeat and hopeful note. After pointing out that "of the 208 [original] trial participants, primary data were available for 190," the study went on to note: "Of the 97 children in the hypothermia group and the 93 children in the control group, death or an IQ score below 70 [evidence of mental disability] occurred in 46 (47 percent) and 58 (62 percent), respectively [at 6 to 7 years after birth]."
Based on that finding the study concluded: "…whole-body hypothermia did reduce the rate of death and did not increase the rates of … severe disability among survivors … These data extend our previous support for the use of hypothermia in term and near-term infants with hypoxic-ischemic encephalopathy."